Low milk supply
Any mum who has struggled to produce enough milk for her baby knows how stressful and heartbreaking this can be. We all want to give our baby the best, and we know breastmilk is it - but what happens when our body just isn't doing what we want it to? There are a number of reasons why we might struggle to produce enough milk for our baby, and many of them can be fixed or easily avoided if you know what to look out for, how to produce a good milk supply and just how your milk supply works!
Causes of low milk supply can be separated into three different categories -
- Pre Glandular – hormonal imbalances due to thyroid disfunction, retained placenta etc
- Glandular – these relate to our breast tissue and how our breasts developed during puberty, or any breast surgery we may have had
- Post Glandular – this is all to do with how our baby is feeding and how effectively they’re signalling our brain to produce milk.
The most common causes we see in mums in the early postnatal period are post glandular - issues with the feeding which are causing a decrease in milk supply, or which have meant mum's milk supply hasn't been stimulated well enough in the first place.
So how does milk supply actually work?
Our little milk making cells are like lightbulbs. During pregnancy our breasts develop more lactocytes (milk making cells) and this is like someone going around fitting light bulbs in all the sockets, these sockets have been 'primed' and the electricity supply connected but we need to switch those light switches on, and this is done through frequent, effective early feeding.
It's crucial for all mums, to ensure your baby is latching deeply, feeding frequently and effectively from that very first feed after birth, so don't hesitate to ask for help if you need it. This helps to ensure all those cells are switched on and producing, rather than laying dormant. After we've primed these cells we need to continue telling our body how much milk our baby needs - and we do this through effective milk removal. Within our milk we have a protein called FIL. This is what's responsible for signalling our brain to tell it how full or empty our breasts are, and therefore how much milk to produce to fill them up again. When we feed baby frequently and they remove milk effectively levels of this protein drop regularly throughout the day. Each time they drop our brain gets a message to say "Hungry baby here, we've just removed x amount, please replace ASAP!" As our breasts fill up with milk, and particularly if this milk is left in our breasts for a long period (even 4-5 hours in the early days) levels of FIL increase. This starts to signal to our brain that we can cut back on production.
Think of your breasts like a supermarket shelf, filled with tins of baked beans. FIL is the supermarket manager. If customers come in regularly throughout the day and clear that shelf of beans, the supermarket manager (aka FIL) sends a message to his supplier each time to order more beans. If, however, someone only comes in once a day to clear the shelf, or people come in regularly but only remove one or two tins, the manager won't order any more, as there's still plenty left on the shelf. So the more frequently you empty your breasts, the more milk you’ll produce. The fuller your breasts remain, the less you’ll produce.
This same theory works if you are expressing breast milk. However this is where we can get into trouble when supplementing with formula. When we add formula into the equation, without compensating with regular milk expression and without dealing with the underlying issue, we're providing food to our baby - without telling our body how much they need. This leads to baby taking less milk at the breast and ultimately decreasing milk supply further. There are some situations when formula is needed, and it's important that this is managed in conjunction with a breastfeeding professional. Each time you’re breastfeeding or expressing your body also releases prolactin, the milk making hormone. These levels spike during a feed and decrease slowly afterwards. The higher your prolactin levels across the day the more milk you'll produce. So allowing baby to feed on demand and ensuring this is frequent enough will cause your body to produce more prolactin and also increase your milk supply.
How can you tell if your milk supply is low?
The following are some signs which may indicate a low milk supply:
- breasts always feeling soft. Not noticing fullness/changes around day 3/4 post birth, and not noticing breasts feeling fuller before feeds and softening afterwards (primarily during the first 3-4 months)
- baby having less than 6-8 wet nappies per day (after the end of the first week, prior to this they should have 1 wet nappy for each day of life)
- poor weight gain or any weight loss
- prolonged feeds of more than 45-60 minutes
- not hearing your baby swallowing or seeing a change in their sucking patterns at the breast after letdown
- baby on and off breast very frequently (every 1-2 hours throughout the day) and not settled in between.
It's worth noting that if you have signs such as poor weight gain, prolonged feeds but your breasts still feel firm after feeds or you've got nipple damage/pain as well it's worth seeking support to improve your baby's latch and also rule out issues such as tongue tie. Many of these signs on their own can be attributed to other feeding issues also, so if in doubt seek some support from a lactation consultant.
Signs commonly mistaken for low milk supply
There are many aspects of feeding your baby which parents often assume means baby isn't taking enough at the breast, but which are actually very normal.
Periods of frequent feeding
Some cluster feeding is normal, particularly around periods of growth spurts. Cluster feeding is defined as a baby feeding frequently (every hour or so) for a period of a few hours, then settling for a reasonable period after. This is common in the evening, particularly around growth spurts.
Only pumping small amounts
How much milk you obtain with a pump doesn't indicate how much is available in your breasts or how much you can produce. A baby's suction is more effective than even the best pumps out there. Particularly if you are using a hand pump or silicone milk collector, these do not have very strong suction and don't give an accurate picture of your milk supply.
Baby taking bottles quickly
Many parents assume that when baby has had a long breastfeed, and then guzzles down a bottle of formula that baby must have been starving, and that their milk supply is low. In actual fact, with most bottles, milk trickles out of the bottle by gravity, without baby even having to suck. When we then lay baby in our arms and place a bottle in their mouth, milk is constantly trickling in, and it's a reflex for our baby to swallow. It's also a reflex for them to suck whenever something is place in their mouth (just like how they'll suck on your finger even when they're not hungry.)
You can optimise your milk production by:
- Ensuring your baby has skin to skin contact and breastfeeds soon after birth
- Hand expressing colostrum when possible during the first few days if baby isn’t latching and feeding well
- Trying to ensure baby receives nothing but breastmilk in the first 6-8 weeks after birth
- Allowing baby to feed as frequently as they demand in the early days
- Offering both breasts at each feed
- Purchasing or hiring a good quality hospital grade breast pump and forming a plan with your lactation professional/IBCLC for implementing expressing if you suspect baby isn't getting enough or you've been advised to top up
- Ensuring your baby is evaluated for complications such as tongue tie early after birth by a qualified practitioner (not all midwives, health visitors, paediatricians etc. have any training in tongue tie assessment so it's worth getting this done by an IBCLC or Tongue Tie Practitioner if you have concerns)
- Keep a close eye on your baby's feeding patterns, nappy output, whether they are actively sucking and swallowing at the breast, and their weight gain/loss
- If your baby requires supplementation use expressed breast milk wherever possible, and consider using methods such as a supply line to provide supplementation whilst also stimulating your milk
Can I take a supplement to increase my supply? What about lactation cookies?
There are a wide variety of herbal, pharmaceutical and food supplements out there which promote themselves as galactagogues (substances which increase prolactin levels and therefore milk production). You may find online information on everything from foods such as oats and brewers yeast, to herbs like fenugreek, milk thistle and moringa. In varying degrees these all work in the same way - by promoting the production of prolactin (our milk making hormone). However increasing prolactin levels is only part of the equation. We need to combine this with frequent and effective milk removal in order to truly increase supply, so no magic pill or supplement will work unless you are effectively breastfeeding or expressing frequently through the day. This is why it's vital to always first assess your baby's latch, and rule out complications like tongue tie. Then optimise their feeding patterns, and ensure you're offering both breasts at each feed. Introducing expressing either after or between feeds, and then consider galactagogues. I would always recommend you speak to an IBCLC before trying galactagogue supplements as some have contraindications with certain medical conditions. Almost all women have the potential to produce a full milk supply for their babies, but often birth practices, poor advice and poor breastfeeding management get in the way of this. If you are concerned about your milk supply, or you're expecting a baby and have had previous issues - seek out some support as soon as possible (even during your pregnancy!) so you have a plan in place to build and maintain a good milk supply from birth.
Low milk supply, breastfeeding, expressing, top ups, formula, increase milk supply, IGT, hypoplasia, PCOS, retained placenta
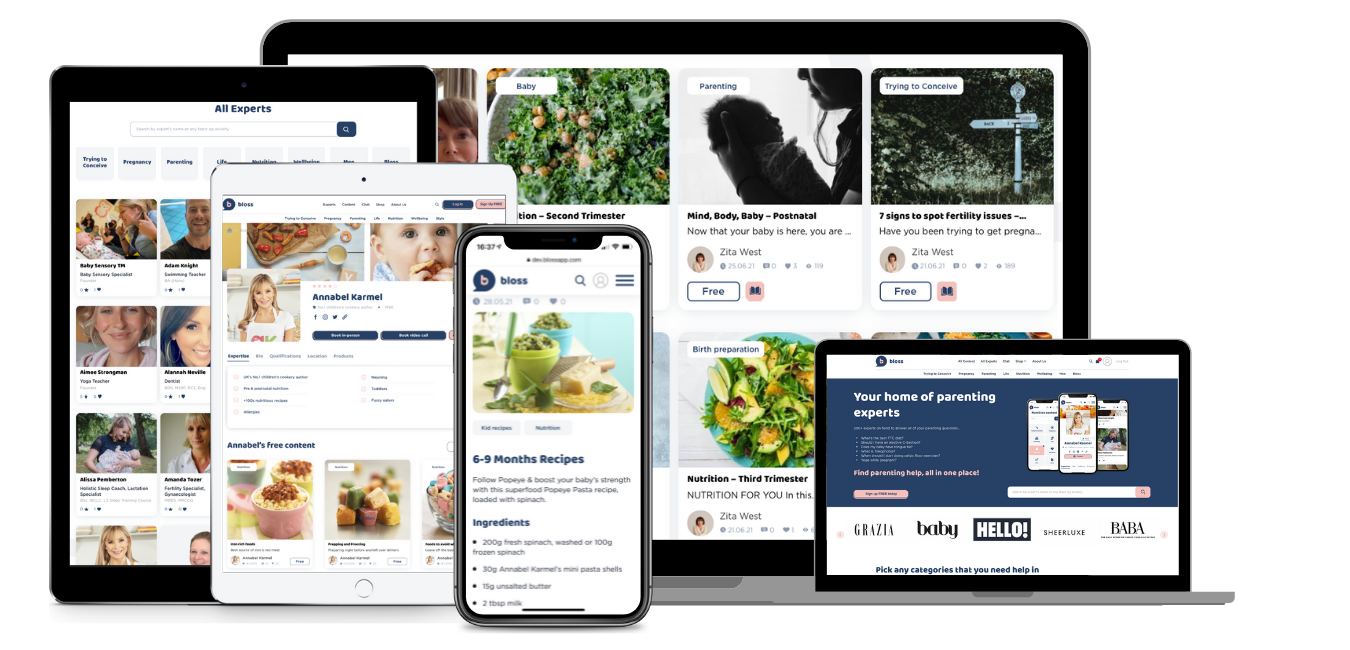
Sign up today for unlimited access:
- Book appointments
- Expert advice & tips
- Premium videos & audio
- Curated parenting newsletters
- Chat with your bloss community
- Discounts & competitions
- Special events




Leave a Rating / Review
You must be logged in to post a comment.